Can Adults Take Vitamin D Drops
Should everyone be taking vitamin D?
(Image credit:
Getty Images
)

Vitamin D is said to help stave off fatigue, depression and even cancer. But some experts argue that for people with healthy levels, supplements are not helpful. What's the reality?
A
As many countries urge populations to stay at home, many of us are paying more attention to our diets and how the food we eat can support our health. To help sort out the fact from the fiction, BBC Future is updating some of our most popular nutrition stories from our archive.
Our colleagues at BBC Good Food are focusing on practical solutions for ingredient swaps, nutritious storecupboard recipes and all aspects of cooking and eating during lockdown.
As many of us find ourselves confined to our houses due to social isolation measures, concerns tend to arise about the lack of sunlight – and possible vitamin D deficiency. For many, a go-to fix is to take supplements.
The supplement, after all, has been touted as a near-miracle. Both vitamin D2 and D3 supplements are available over-the-counter without a prescription and have been linked to improving immunity, tiredness and muscle weakness, bone pain, and depression. They've also been said to help stave off cancer and the consequences of ageing.
You might also like:
• Why vitamin supplements don't work
• The world's most nutritious foods
• What I learnt by living without artificial light
But the debate over whether all adults need to take vitamin D supplements is contentious.
Few doubt the role that vitamin D plays in our bone health to regulate calcium and phosphate in the body, which is why those who have a vitamin D deficiency are particularly encouraged to address it. And that may be more people than you think: one study estimates that around 20% of the population in the UK has a profound vitamin D deficiency, for example.

A third of UK adults who supplement their diet with vitamins take vitamin D (Credit: Getty Images)
But some experts say that people with healthy levels have no need of vitamin D supplements – which would be most people. In other words, they argue that in healthy people, vitamin D is not, as some have hoped, a way to prevent disease.
So what's the reality?
The basics
Despite its name, vitamin D is not a vitamin. Instead, it is a hormone that promotes the absorption of calcium in the body. The challenge is that, aside from a few foods like oily fish, vitamin D is hard to find in the average diet. But in the presence of "ultraviolet B" rays, our skin can produce its own from a common cholesterol.
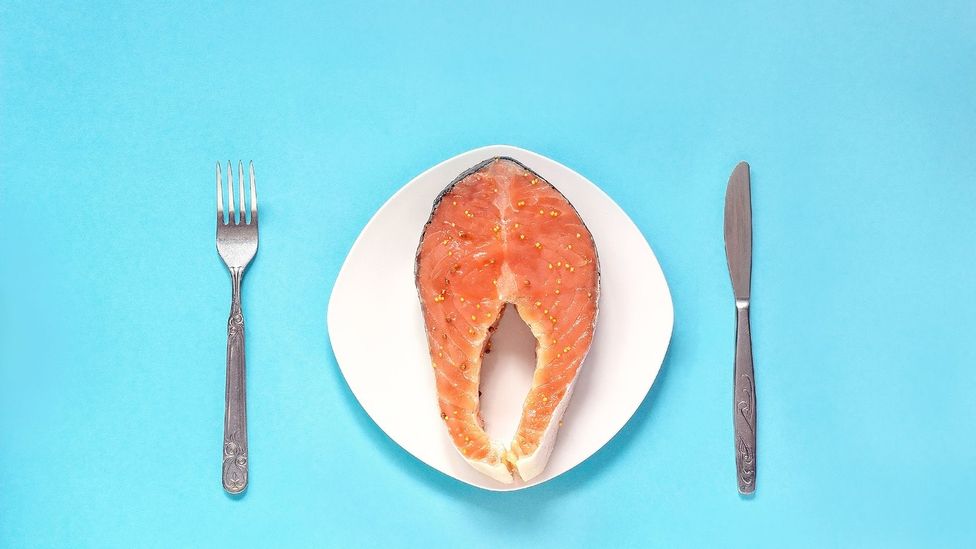
Vitamin D is found in only a few foods, like oily fish (Credit: Getty Images)
There are two main types of D. The first is vitamin D3, which is found in animals including fish and is the kind the skin makes when exposed to sunlight. The second is vitamin D2, which comes from plant-based foods including mushrooms. Studies have found that D3 is more effective, and the conclusions of a 2012 meta-analysis argue that D3 is the preferred choice for supplementation.
Today, the UK's Public Health England (PHE) recommends every adult takes a 10-microgram supplement in autumn and winter, when the angle of the sunlight hitting the earth prevents as many UVB rays from penetrating the atmosphere. The government body also recommends that those at risk of lower vitamin D levels, including people with darker skin, take a supplement year-round.
Other countries follow similar guidelines. In Canada, adults are advised to get 15 micrograms of vitamin D and have two servings of vitamin-D fortified milk or soy alternatives every day, while cow's milk and margarine must be fortified with vitamin D by law. In the US, adults also are advised to get 15 micrograms, while much of the country's milk, breakfast cereals, margarine, yogurts and orange juice is fortified, too.
Those guidelines and fortification efforts came about largely in an attempt to fight rickets in the mid 20th Century. We know that low vitamin D levels reduce the body's levels of calcium, which leads to a decrease in bone density and can cause rickets, particularly in babies and children.

In countries including the US, Canada and UK, foods like cereal and milk often are fortified with vitamin D (Credit: Getty Images)
However, that advice has recently been expanded up, at least by the Association of UK Dieticians, in light of self-isolation during the current pandemic. In a post released in March 2020, as the UK entered spring, it said: "If you are having to self isolate or if you are unable to go outside, you should consider taking a daily supplement containing 10 micrograms to ensure a healthy vitamin D status (for adults and children over the age of one)."
We know that low vitamin D may cause muscle weakness and fatigue. One study found that low vitamin D was high among people with fatigue and that their symptoms improved after five weeks of vitamin D supplements, while a small study from Newcastle University found that low vitamin D could cause fatigue as low levels cause mitochondria, the 'power stations' in every cell of the body, to be less efficient. Studies of cancer patients have found similar effects. Vitamin D may also help bolster and regulate the immune system by clearing bacteria.
Broken bones
But vitamin D's importance doesn't necessarily mean people with healthy levels of vitamin D require supplements. Consider one of the most common reasons for supplementation: bone growth and maintenance.
The current guidelines on how much vitamin D to take were informed by research involving the elderly population living in care homes, who don't get as much exposure to the sun and are more prone to fractures and osteoporosis than the general population. But Tim Spector, professor of genetic epidemiology at King's College London, has argued that such studies are "probably flawed".

One common reason to take supplements is to promote bone strength, but the evidence behind this isn't clear-cut (Credit: Getty Images)
It's true that the evidence isn't clear-cut. One meta-analysis published in August 2018 concluded that increasing the levels of vitamin D in the general population is unlikely to decrease the risk of bone fractures in healthy people. And a meta-analysis of 81 studies found that vitamin D supplementation doesn't prevent fractures or falls, or improve bone mineral density. The researchers concluded that guidelines should be updated to reflect this.
But Sarah Leyland, osteoporosis nurse consultant at the National Osteoporosis Society, says vitamin D supplements may be useful for at-risk groups who don't get any sunlight exposure. According to the NHS, people only need to be outside for a short period of time, with hands and forearms uncovered and without sunscreen, to get enough vitamin D between March and October.
"We know that healthy people living in the community won't reduce their fracture risk by taking calcium and vitamin D supplements," Leyland says. "However, people who may not be getting enough – such as those who are housebound or live in sheltered accommodation – can benefit from these supplements."
Still, researchers haven't found clear evidence of that, either. One meta-analysis examining the prevention of fractures in community, nursing home and hospital inpatient populations concluded that vitamin D alone is unlikely to prevent fractures in the doses and formulations tested so far in older people. And some evidence suggests that high doses can actually result in an increased number of fractures and falls. One randomised study found that high-dose monthly vitamin D supplements increased the risk of falls among the elderly population by 20-30% compared to those on a lower dose.
D for disease
There is also conflicting research on the relationship between vitamin D and other diseases, even ageing.
One main claim is that vitamin D supplements will boost the immune system. Adrian Martineau, professor of respiratory infection and immunity at The London School of Medicine and Dentistry, Queen Mary University of London, who leads a research group on the effects of vitamin D on health, has found that vitamin D plays a role in improving respiratory infections.

One study found that vitamin D helps decrease the risk of respiratory infections – though only slightly (Credit: Alamy)
When his team analysed raw data from 25 clinical trials involving 11,000 patients from 14 countries, they found a small benefit to taking daily or weekly vitamin D supplements to reduce the risk of respiratory infections, asthma attacks and bronchitis. Although the paper soon attracted robust criticism, Martineau points out that the reduction of risk, while slight, is still significant and comparable to the effects of other health measures: to prevent a single respiratory infection, you'd have to give 33 people vitamin D supplements – compared to, for example, giving a flu vaccination to 40 people to prevent a single case of flu.
Or take ageing. One paper looking at the link between vitamin D and life expectancy found that vitamin D3 can help with protein homeostasis – the process by which proteins are regulated within cells to maintain their health. "Our observation that D3 improves protein homeostasis and slows ageing highlights the importance of maintaining appropriate vitamin D serum levels," the researchers write.
But other studies have been less conclusive. One meta-analysis concluded that more research is needed to clarify the effect of vitamin D on mortality. The link between cardiovascular disease and vitamin D also has yet been properly established: the link could mean that heart disease is causing low vitamin D levels, not the other way around.
Correlation or causation?
This is an issue with nearly all of the studies that link low D to diseases.
Ian Reid, professor in medicine at the University of Auckland, believes that diseases cause low vitamin D levels, as being unwell often leads to spending less time outdoors exposed to sunlight, rather than vice versa. "If you take any group of patients with almost any disease, their vitamin D levels will be lower than in a healthy individual. This has led some to hypothesise it's low vitamin D developing the disease, but there's no evidence to prove it," he says.

Some experts believe people who are unwell have low vitamin D levels because they spend less time outdoors, not that their low levels cause health problems (Credit: Getty Images)
Researchers have found that higher vitamin D levels are associated with a lower risk of colorectal cancer – it plays a role in stemming the formation of new blood vessels and stimulating better communication between cells. Vitamin D also has been found to help maintain normal levels of calcium in the colon, which slows growth of non-cancerous but high-risk cells.
Other studies, including of the link between vitamin D and liver cancer, breast cancer and prostate cancer, suggest there is good reason to think that low vitamin D plays a part in the spread of cancer cells. But taking supplements would then, surely, help stave off cancer – and a recent meta-analysis failed to find that supplementation reduced cancer risk.
"This is likely to be a two-way street, with cancer causing vitamin D deficiency by affecting vitamin D metabolism, dietary intake and sun exposure, and vice versa via anti-proliferative effects of vitamin D. The two hypotheses are not mutually exclusive," says Martineau.
D for depression
Another oft-discussed condition is seasonal affective disorder (SAD), a mood disorder caused by the seasonal drop in exposure to sunlight. The link between light exposure and SAD is long-established. But again, a direct link to vitamin D has been difficult to prove.
Evidence suggests there may be a relationship since vitamin D is associated with levels of both serotonin, important for mood regulation, and melatonin, which regulates our sleep. Low levels of either hormone could contribute to SAD symptoms. Researchers have yet to carry out a definitive randomised control trial, however, and the exact mechanism by which vitamin D bolsters the hormones is unknown. One theory is that vitamin D receptors – which are found in many parts of the brain and concentrated in the hypothalamus, a region involved in our circadian timing – play a part in controlling the body's hormone levels.
Research has found that vitamin D plays a wider role in our mental health, from depression to schizophrenia, as well as in brain development, but how it plays a role also remains unclear. A meta-analysis published earlier this year found that while there is a correlation between lower vitamin D levels and depression, that didn't necessarily mean D caused depression.
Again, perhaps depressed people just went out less and got less sunlight.
Sunshine serum
If studies are inconclusive, though, perhaps that doesn't reflect on the importance of vitamin D. Perhaps it's the fact that most of them are based on supplements, not sunshine.

Some experts believe that vitamin D is most effective when it's from the sun, not supplements (Credit: Getty Images)
Some scientists argue that getting vitamin D from supplements isn't as effective as getting it straight from the sun, as the process that happens before the body makes vitamin D from sun exposure is more beneficial. More conclusive research around this is currently underway.
Even so, most experts generally agree that even vitamin D supplements can benefit those who have very low levels. Martineau says his research found that those with low levels of vitamin D tend to see the most benefits of supplementation preventing respiratory infections, whereas the effects are a lot more modest when levels are moderately low.
Reid says his studies have also shown benefits in those with low levels. But as most people have vitamin D levels above that threshold, they wouldn't see benefits from supplementing.
The trouble is that it can be difficult to predict who is at a highest risk of suffering from low vitamin D. As medical historian Roberta Bivins of the University of Warwick points out, the amount of vitamin D a person stores, and therefore requires over winter, isn't just dependent on skin tone and the amount of time a person spend outdoors.
"It's very individual how much sun exposure a person needs during summer, depending on the pigment in the skin to the amount of fat in the body and how quickly your body makes new bone. It's incredibly complicated," she says.
That's why the best way to determine if you have low vitamin D is not by symptoms alone, but with a blood test arranged through your medic.
Supplement levels
Then there is the question of exactly what level of supplementation people need. Reid says there's "no danger" in taking over-the-counter vitamin D of less than 25 nanomols per day.

US and Canada guidelines suggest taking 15 micrograms of vitamin D supplements each day, but some believe it's not enough (Credit: Alamy)
But with supplements offering doses as high as 62.5 micrograms available over the counter, there are concerns around the risk of excessive vitamin D levels, which can, in rare cases, cause side effects, including nausea and vomiting. In the long term, some studies suggest too much vitamin D can increase risk of cardiovascular disease, although the research isn't conclusive.
But others argue that even more vitamin D is needed.
In 2012, chief medical officer Sally Davies wrote a letter to GPs urging them to recommend vitamin D supplements to all at-risk groups, writing that a "significant proportion" of people in the UK probably have inadequate levels of vitamin D. In June 2018, researchers from the University of Birmingham's Institute of Metabolism and Systems Research wrote that the death of a baby from complications of heart failure caused by severe vitamin D deficiency, and the serious health complications of two others, was just the "tip of the iceberg" in vitamin D deficiencies among those at risk.
Suma Uday, co-author of the paper and PhD doctoral researcher at the university, says these deficiencies occur because infant vitamin D supplementation programs are poorly implemented in the UK and not monitored. "In the infants we describe, deficiency occurred because infant vitamin D supplementation was not recommended or monitored. Any infant devoid of vitamin D for prolonged durations can develop low calcium levels, which can result in life threatening complications such as seizures and heart failure," she says.
With such conflicting results, it's unsurprising that medical experts themselves are deeply divided over the benefits of widespread supplementation. Some even argue that vested interests are propping up the billion-dollar vitamin industry, with Spector calling vitamin D supplements a "pseudo-vitamin for a pseudo-disease".
While the debate continues, many experts are looking to Brigham and Women's Hospital, an affiliate of Harvard Medical School in Boston, whose researchers are carrying out a long-awaited randomised trial, VIital, to investigate whether supplementation of vitamin D and omega 3 has any effect on cancer, stroke and heart disease in 25,000 adults.
It's hoped that these results, expected to publish later this year, will bring the debate closer to being resolved. In the meantime, it's widely agreed that vitamin D supplements, especially over winter, will be a waste of money at worst.
Disclaimer
All content within this column is provided for general information only, and should not be treated as a substitute for the medical advice of your own doctor or any other health care professional. The BBC is not responsible or liable for any diagnosis made by a user based on the content of this site. The BBC is not liable for the contents of any external internet sites listed, nor does it endorse any commercial product or service mentioned or advised on any of the sites. Always consult your own GP if you're in any way concerned about your health.
--
Join 900,000+ Future fans by liking us on Facebook , or follow us on Twitter or Instagram .
If you liked this story, sign up for the weekly bbc.com features newsletter , called "If You Only Read 6 Things This Week". A handpicked selection of stories from BBC Future, Culture, Capital, and Travel, delivered to your inbox every Friday.
Can Adults Take Vitamin D Drops
Source: https://www.bbc.com/future/article/20181010-do-vitamin-d-supplements-work

0 Komentar